Access to healthcare services in New Mexico has, in many cases, not improved, and the burdens on the state’s Medicaid have increased in recent years, according to a new report.
Staff from the Legislative Finance Committee discussed the findings from the 2025 Medicaid Accountability Report with state lawmakers on Tuesday during an interim committee meeting in Hobbs. The biannual report examines the effectiveness of the state’s Medicaid program and its effectiveness as it relates to the state and its ability to deliver quality services.
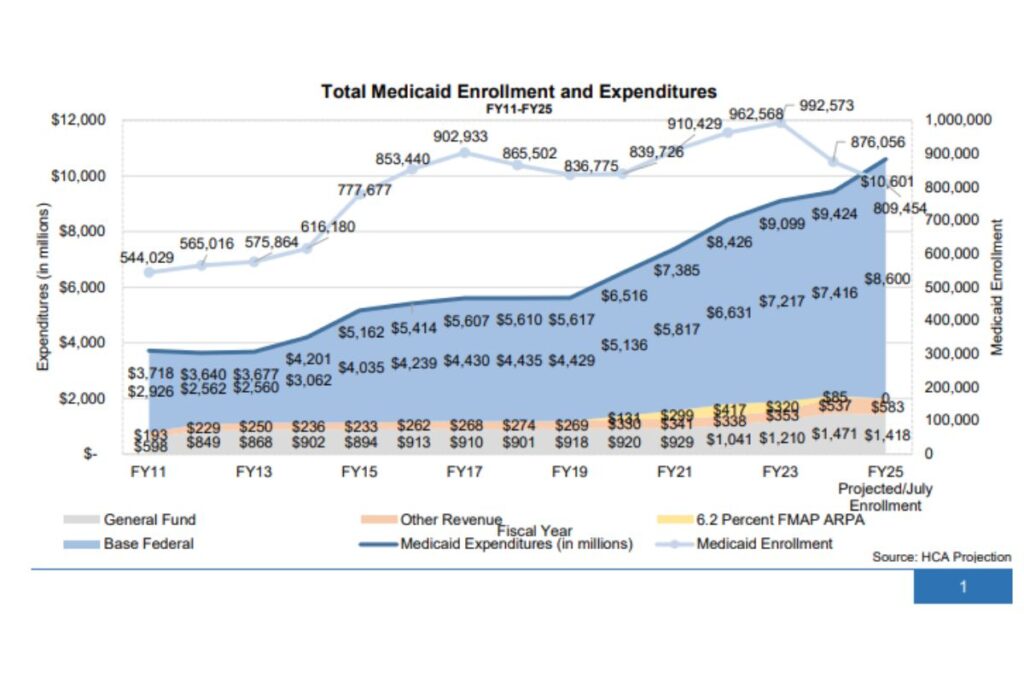
Over the last three years, the state has invested billions in its Medicaid program, including $2.2 billion for rate increases to Managed Care Organizations. According to the Center for Medicare & Medicaid Services, managed care is a system that delivers health services through contracts between the state and private health plans known as Managed Care Organizations. Those organizations are paid a monthly per-member payment, also known as an MPMP, by the state to provide care to Medicaid recipients.
But Allegra Hernandez, senior fiscal analyst with the Legislative Finance Committee, said that infusion of money has not translated into easier access to many types of care.
“Despite significant investments that you all, as the legislature, have made in behavioral health and in Medicaid more broadly, the systems are not improving for users in the way that we would expect and hope with these investments, and moreover, spending has increased significantly, and these payoffs are not yet demonstrated to have shown up,” she said to lawmakers.
The report found that expenses associated with Turquoise Care, the state’s Medicaid managed care program, have jumped from $9.09 billion to $11 billion since FY 23, even as the number of New Mexicans on Medicaid is 31,000 less than it was in 2016.
Elsewhere, the report found that New Mexico is paying more to provide health services. The report showed that New Mexico has higher rates than neighboring states, up to 186% for physical health services and 325% higher for behavioral health services.
In New Mexico, the number of behavioral health providers has shrunk. Between 2022 and 2024,
New Mexico lost 1,082 prescribing and 427 non-prescribing behavioral healthcare providers.
“That is possibly due to some unwinding of the public health emergency (related to COVID-19), the reduction in telehealth, but the vast majority of counties, except for Cibola County, saw a decline in prescribing providers,” Harry Rommel, a fiscal analyst for the Legislative Finance Committee, said to lawmakers.
Rommel added that a George Washington University study shows that in New Mexico, some primary care practitioners could be filling the gap in prescribing providers. He said that the study shows that in New Mexico, several primary care providers are prescribing nearly a dozen behavioral health prescriptions per year.
The share of people who go to an emergency room for behavioral health issues and then receive a follow-up call seven days later has also fallen from 37% in 2022 to 31%, Hernandez said.
A secret shopper survey conducted in August was also mentioned in the report, which indicated that where access to care is available, it is a challenge to get in to see a doctor. The survey found that on average, it took six to seven calls for a new patient to book an appointment with a primary care physician and 14 calls to schedule an appointment with a behavioral health physician. Those numbers were the same as those from a similar survey conducted in 2023.
Survey respondents who were able to schedule an appointment after completing paperwork online or in person were offered an appointment 15% of the time to a primary care provider and six percent for a behavioral health provider.
Rommel noted there was one flaw with the survey, given that more providers, such as UNM Presbyterian, have adopted a policy where a person must either come in person to complete a patient profile or do so using a patient portal before an appointment is scheduled.
“That is just one slight problem with the secret shopper survey is that…we don’t have a way to adapt to that new policy that some of these health care providers have implemented,” he said.
