“It’s a sea change.”
That’s how Sylvia Villarreal, CEO and owner of Taos Clinic for Youth, described telemedicine and its place in rural healthcare. Villarreal has offered limited telehealth services, also referred to as telemedicine, to patients for about eight years.
Telehealth refers to healthcare services that are administered remotely between patient and doctor, typically over video using a broadband connection. In theory, telehealth could significantly expand access to healthcare in rural communities. But implementing telehealth across the U.S. has proved challenging for a number of reasons — insurance coverage and reimbursement being one of the larger roadblocks to adoption for providers.
After a recent push at the federal level to expand telehealth service reimbursements for Medicaid and Medicare patients in response to COVID-19, one of the biggest challenges to adoption has suddenly been removed. And local providers are seeing the impacts immediately.
Telehealth is a boon to rural healthcare
Rural communities across the U.S. are facing a healthcare access crisis. Rural areas tend to have fewer healthcare providers, and residents typically must drive further distances to reach those providers, introducing a host of difficulties to accessing healthcare that urban residents don’t usually face. In New Mexico, nearly all of the state’s 33 counties have portions that are designated as “medically underserved,” according to the U.S. Health Resources and Services Administration.
Telehealth services can offer a number of benefits to rural communities, including reducing transportation costs, Villarreal said. That’s especially important when patients need to see specialists or subspecialists who might not be available in their area.
In 2012, Villarreal began offering telemedicine services for her patients who needed to see subspecialists at UNM Health Services.
“For many of our kids, it’s difficult for them to get transportation, or get in a car for two or three hours to get to an appointment,” Villarreal said. Using a video telemedicine platform, a family can instead drive to the local clinic, sit down with their familiar doctor, and go through the consultation with the specialist.
“The patient would be seen, we’d get their vital signs done, and the subspecialist could then look in a patient’s electronic record to see past history or growth charts or labs, that kind of thing,” Villarreal said.
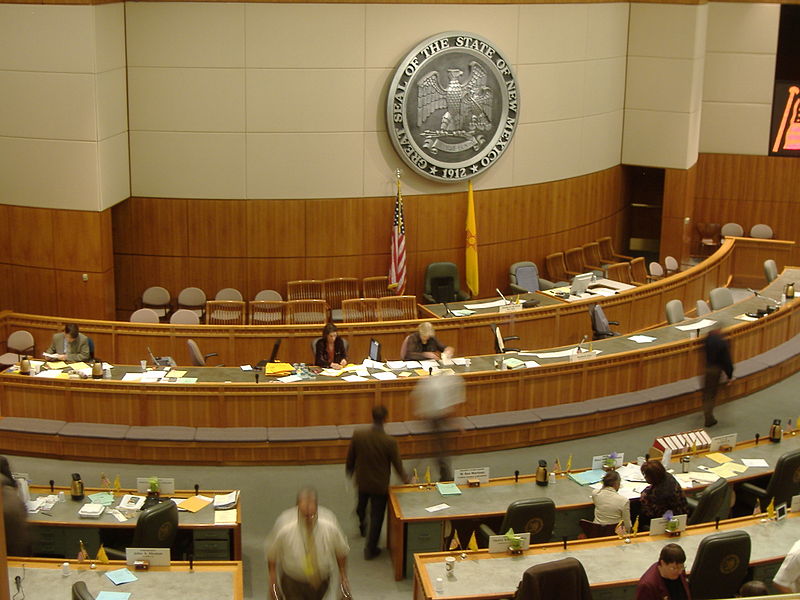
New Mexico has in some ways become a pioneer in telehealth, said Beth Landon, chairperson of the New Mexico Telehealth Alliance, a 501(c)(3) based in Albuquerque. In 2019, the state Legislature passed SB 354, “which gives New Mexico one of the most progressive telemedicine laws in the country,” Landon said.
The bill established both coverage parity, meaning that private insurers operating in the state must cover telehealth services the same way it covers in-person services; and payment parity, meaning the doctors must be reimbursed for telehealth services at the same rate as they would be for in-person services. The bill also removed geographic barriers for coverage, opening up telehealth services to patients living in urban and rural areas alike.
“A psychiatrist in eastern Albuquerque can provide via video care to an in-patient on the westside of Albuquerque, and we don’t have to pay for an hour of that psychiatrist’s time for driving,” Landon said.
There are still plenty of roadblocks to widespread adoption of telehealth among rural residents and healthcare providers. Broadband availability, which is a requirement for all telehealth services, is lacking in many rural parts of the state. The cost of telehealth software, which must be fully encrypted and HIPAA-compliant, can pose another challenge to rural clinics that are operating in the margins financially.
“We don’t have broadband everywhere, providers don’t have the resources to purchase equipment that’s necessary to do this, and there are rules for some providers that have not been able to do it,” explained Joie Glenn, an executive committee member at NM Telehealth Alliance and former executive director of the New Mexico Association for Home and Hospice Care.
And while private insurance providers have begun expanding telehealth service coverage and reimbursement, the federal Medicaid and Medicare programs have been slower to embrace the new healthcare medium.
Telehealth and COVID-19
Before March 2020, the U.S. Centers for Medicare and Medicaid Services (CMS) only offered reimbursement for certain types of telemedicine — specifically, clinic-to-clinic services, such as those Villarreal offers to her patients meeting with UNM Health Services specialists. That meant doctors would not be reimbursed for in-home telehealth appointments, in which patients use video software to connect with a doctor without leaving the house.
But as the COVID-19 outbreak swept across the country, telehealth emerged as a crucial tool in slowing the spread of the disease, according to U.S. Rep Xochitl Torres Small.
Torres Small, a Democrat, has pushed for an expansion of telehealth in rural New Mexico during her time in Washington D.C. She and other members of Congress urged the U.S. Health and Human Services Department, which oversees CMS, to tweak the rules around telehealth coverage in response to COVID-19.
“We’ve been working before COVID-19 to expand reimbursement for telemedicine, but in this crisis, we’ve expanded it significantly,” Torres Small told NM Political Report. “It’s helping address the preparedness challenge for COVID-19 in crucial ways. The more services that can be provided at home, the more we can make sure that we’re continuing to keep patients safe and healthy, that they’re not getting sick based on chronic conditions or other challenges while we’re trying to keep the clinics clean and try to stop the spread of COVID-19.”
CMS is now reimbursing healthcare providers for in-home telehealth services, in which a patient can stay at home and connect with a doctor online. CMS has also expanded the definition of telehealth to include phone calls, rather than video-only appointments.
That’s critical for rural families who may not have access to video platforms, a problem Villarreal said she’s run into at her clinic in Taos.
“Many of our families don’t have technology, so they don’t have a computer, they don’t have internet, and many of their phones are not smartphones,” Villarreal said. “Now we have the possibility of me talking to a family at home, and if they don’t have technology, I can talk to them on the phone.”
CMS has also relaxed rules around healthcare providers using video software that is not HIPAA-compliant. Glenn said that change, coupled with the social distancing initiatives, has forced some patients who might otherwise shy away from telehealth to try out the services.
“People are becoming more and more accepting of the technology, and now folks are hesitant to go into their provider settings to take care of their chronic disease, or can’t go there, so a lot of them are initiating it telephonically, and they work into the video,” Glenn said.
There are still some kinks that need to be addressed at the federal level to make access to telehealth services equitable, Torres Small said, pointing to rules that prevent federally-qualified health centers in rural areas from providing phone telehealth services. Private clinics, on the other hand, can be reimbursed for telephonic telehealth.
“The person who needs the prescription refill doesn’t know the difference between a federally-qualified health center and a private clinic. But some patients can get that telephone consultation, while others don’t,” Torres Small said. “Both of those communities need that support, because there are areas within those service networks where people don’t have access to good, reliable internet, and they [still] need that service.”
Still, the expansions made in response to COVID-19 are a step in the right direction, Glenn said.
“COVID has helped this in a number of ways, for people to access this medium and really recognize the benefits of it. We’re kind of riding this wave in a real positive way, given the negative circumstances,” Glenn said.
Villarreal agreed.
“You can’t put the genie back in the bottle. The future of medicine, with Medicaid, is the ability to talk to families at home,” she said.